
2023 Maryland Hospital Safety Ratings Released
In the spring of 2023, The Leapfrog Group, a nonprofit healthcare watchdog, released hospital safety grades for 35 hospitals in Maryland, with several receiving top marks for patient safety.
D'Amore Personal Injury Law, LLC
Serious Injury Lawyers Proudly Serving
Baltimore, Annapolis, & Washington, D.C.
Both the Health Insurance Portability and Accountability Act of 1996 (HIPAA) and the Health Information Technology for Economic and Clinical Health Act of 2009 (HITECH) created incentives for U.S. health care providers to improve medical recordkeeping and information sharing by transitioning to electronic health records (EHR).
Both of these Federal Laws encouraged the adoption and meaningful use of health information technology, with the goal of lowering the number of patients harmed by avoidable medical errors.
Unfortunately, like any sweeping change, the adoption of new EHR technology has not gone over without a hitch. The cash incentives provided by the Government to health care providers, and the Medicare and Medicaid reimbursement penalties for non-compliance, have created an overwhelming demand for EHR computer systems and software platforms.
This, in turn, has opened up a multi-billion-dollar industry, with many companies competing for business. Healthcare providers are free to choose their own EHR systems, and not all EHR platforms are created equal. The unfortunate and unintended result has been a rise in malpractice claims involving EHR use that caused or contributed to a patient’s injuries.
An October 2017 study by a major medical practice insurance company found that between 2007 and 2010, only two medical malpractice claims involving electronic health records were filed. However, between July 2014 and December 2016, there were 66 such cases filed.
Understanding the Rise in EHR-Related Malpractice Claims
A 2010 article in the New England Journal of Medicine explored four “core functionalities” of EHR systems and the malpractice liability risks most common to each.
Documenting Clinical Findings
As with conventional paper records, failures in charting, incomplete charting, or charting errors still occur and may continue to play a role in medical malpractice cases. One of the specific risks of EHR systems is the “copy and paste” function. Without certain safeguards, this function creates an increased risk of “cross charting”. This occurs when a provider thinks he/she is “pasting” information into a new section of the patient’s chart, but he/she has unwittingly opened a different patient’s chart and pasted the information into it erroneously.
In 2014, I saw this problem first hand. I represented a young boy admitted to a major metropolitan hospital for a complex neurological condition. His medical issues required the staff taking care of him to have an extremely detailed understanding of his hourly medication levels and his physiological response to each. This knowledge needed to be communicated between several specialists, and all of his nurses over the course of several days. Many of his providers saved time by using the “copy and paste” function while inputting his chart data. Eventually, the critical information needed to make emergent decisions for this young boy got lost in the shuffle, and he suffered terrible and tragic consequences.
When we obtained the child’s medical record, we were in shock. Paragraphs of information from other patients were imputed and over struck. There was so much duplicative, erroneous and stale information, we had to physically cut the pages with scissors and tape them together to create what should have been the child’s contemporaneous chart. One of the expert witnesses hired by the hospital to defend the case even admitted in deposition that he could not understand the actual patient records, and had to rely on an outline prepared by the hospital’s lawyer to understand the child’s treatment timeline.
While we were able to successfully settle the case, this tragedy should never have occurred. Additional training of the staff in the use of the EHR and built in safety mechanisms in the software can, and should, be used to avoid these types of events.
Recording Clinical Findings, Test and Imaging Results
While EHRs make it easier to record and transmit test and imaging results, they also place additional responsibilities on doctors, who are responsible for the medical information they access. Teaching “old dogs new tricks” is not the easiest of tasks. Health care providers who are used to doing things “the old way” may miss information when it is presented by an EHR system in a new and unfamiliar format.
At our firm, we just recently encountered this very issue. Below is a basic growth chart that pediatricians have been filing out for decades. The information recorded on the chart allows for a quick analysis of how a baby’s body is growing, how his head is expanding and how he is gaining weight during the first two years of his life. The chart allows for a quick and easy to to comprehend and assess these very important data points. Variants in these data points can be red flags for severe, but treatable diseases.
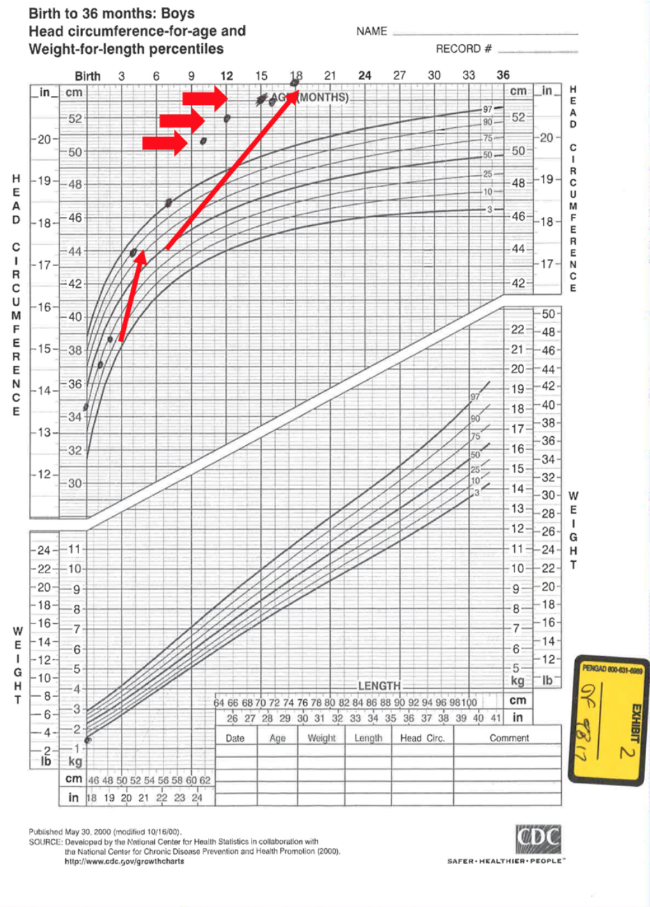
Notice the first red arrow on the lower left. It shows that the child’s head circumference has jumped over 4 growth curves in just three months. The larger bold arrows in the upper right show that by 9 months, the child’s head size is literally off the charts. Over the next 9 months, his head continues to expand beyond the pale of any known growth curve.
Tragically, this child’s doctor never recognized his abnormal head growth, and the child ended up suffering permanent brain damage. How could the doctor have missed something so obvious? Perhaps it was because for the first forty years of his career, the doctor saw the information presented just like you see it above. However, in this case, the hospital had switched to an electronic medical records system. This same information was available to the doctor, but it looked like this:
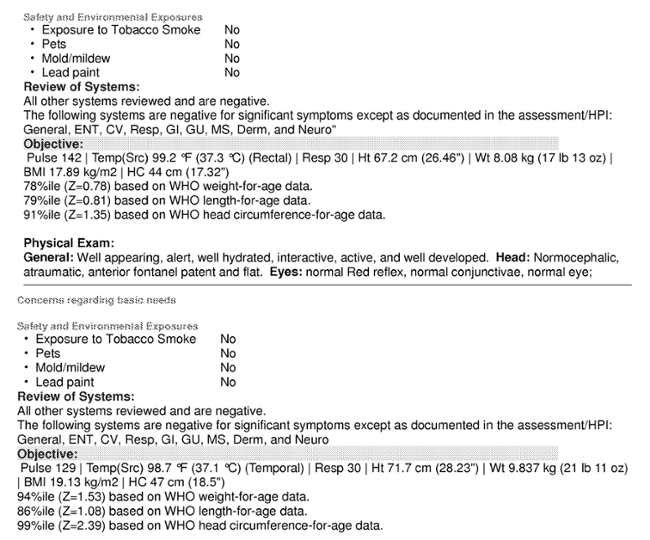
From what we were able to ascertain during the lawsuit, the doctor never had access to “head growth charts” within the EHR, and the EHR system wasn’t designed to “flag” abnormal growth patterns. Not surprisingly, we were able to obtain a significant (but confidential) settlement for this little boy.
Entering Orders
Entering orders, prescriptions, and similar documentation into an EHR has become a widely-accepted practice; one report from The Doctors Company estimates that over 80 percent of office practices now use their EHRs for entering orders. However, the report also estimated that 10-15 percent of electronic orders contain errors, about 33 percent of which are potentially harmful. As with electronic test and imaging results, failure to act on information available in an electronic order system creates potential risk of harm to patients.
Supporting Clinical Decisions
EHRs offering Clinical Decision Support (CDS) capabilities must be certified for compliance with Meaningful Use requirements. However, because ultimate responsibility for content rests with the provider, doctors and hospitals must carefully consider whether the CDS aligns with the provider’s or patient’s needs. In addition, most software vendor contracts attempt to shift all liability for CDS use onto the physician, while some malpractice policies exclude coverage for product liability or indemnification of third parties, including software vendors.
The most recent study from The Doctors Company examined 66 claims made between July 2014 and December 2016, and it compared them to the results of an earlier study examining claims made between 2007 and June 2014. Comparison of the two studies revealed the following patterns:
The move towards implementation of EHR systems creates a combination of potential system errors and potential user errors that should be concerning for patients. Therefore, it is important to understand your medical condition and how it is being treated. This will help protect you from some of the mistakes we have discussed in this article. Never be afraid to ask questions. Doctors and nurses are human, and humans make mistakes. And humans who rely on bad information from machines make mistakes without even knowing it.
Dealing With EHRs in Your Malpractice Case: Some Tips
EHR issues are cropping up in medical negligence cases more and more. If you suspect you or loved one has been the victim of medical malpractice, you should ensure you are working with an attorney who understands these important issues.
When building a case involving claims of medical malpractice related to electronic health records, your attorney should consider:
If you or a loved one have suffered because of someone else’s negligence, contact us immediately.
Fill out the form below and we will contact you.
Or, give us a call at

In the spring of 2023, The Leapfrog Group, a nonprofit healthcare watchdog, released hospital safety grades for 35 hospitals in Maryland, with several receiving top marks for patient safety.

Maryland has some of the best medical facilities in the nation. But not every hospital is up to par. In

What Is the Difference Between a Birth Defect and a Birth Injury? When your child faces medical issues at birth,